Why Gamify Health Care? Why Not Healthify Blockbuster Games?
Ayogo doesn’t ask why gamify health care but why not instead “healthify” blockbuster games? It’s an interesting twist to the current trend of ‘gamifying’ everything, from the number of steps we take each day to making better choices in our diet. At Ayogo, a Vancouver B.C. mobile gaming company, they believe games can be used as effective tools for motivating and educating the common person, like me! The thought behind this is that if we want to get people to do the things they need to do, the best way to get them to do it is to make it playful.
Playful! Hear that health care?? We want to PLAY and have FUN!!!
There seems to be a growing trend for game developers to not only to entertain folks using console & social networks, but to create game apps for the health sector. Ayogo’s slogan is very cool too, building “Games for Good”! Whodathought that gaming could be so good & healthy for you 10 or even 5 years ago!
Noninvasive Skin Sensor Technology for Future Healthcare Monitoring
New skin sensor technologies are being developed and this video demonstrates how a small tattoo like this device can be applied like a band aid! It would read and transmit electrical input and collect data of that patient for doctors to monitor remotely.
Laws & regulations surrounding the evolution of Telemedicine
Where is telehealth heading?
The speakers at the InformationWeek Healthcare’s IT Leadership Forum agree that complete access for patient information and more exchange between patient and care giver are in our future.
“If there’s one thing that’s going to revolutionize healthcare, whether it’s IT, ACOs, or any aspect of health reform, what you’re going to see is patients taking back healthcare from their providers,” states Neil Calman, MD, the CEO and co-founder of the Institute for Family Health. “You’re going to see patients who want complete and unfettered access to their medical records. Forget all this where we’re going to keep the data to ourselves for seven days before it’s released to patients, or we’re going to create models of abstracted data to give to people. They will have total and complete, instant access to their medical information, whenever, in multiple formats, however they want it.” Under the HITECH Act we will see more accessibility to access to our health records, but establishing and maintaining a secure web portal which would allow access for the patient to exchange data on file has many complications. I hope to see more advances in electronic health records which would allow users to directly enter their own data or possibly share data with their loved ones and caregivers. Monitoring health will no longer be a passive event. Correlation to patients active involvement (and with graphic visualization of feedback) is important if change of behavior is the desired outcome.
Microsoft HealthVault (and Google’s now defunct Google Health) are patient portals where their sensor data can be stored and later accessed by the user and their healthcare professional to monitor chronic disease. HealthVault vendor Akevelon recently joined the mobile bandwagon and released a health app for their the Windows phone which synchs up with records on file and displays data (also includes social media shares in case you desire to let the world know that you’ve lost weight, lowered your blood pressure).
Regulatory Issues – Crossing the border & the state of Washington
Typically, healthcare professionals need to obtain a state medical license in the state where they wish to practice, yet with the emergence of telemedicine, there is no clear law resolving the question of “where care actually occurs”. The patient and the health care provider may be in different states. Questions arise whether care is legally provided at the location of the patient or at the location of the practice.
The Center for Telehealth and e-Health Law (CTeL) has created an interactive map, to review each states’ regulatory license, just click on the map to learn about your jurisdiction.
Washington state has no rules or laws on telemedicine, but the following general guidelines:
Who’s not required to follow HIPAA & why it’s so important to go after those who violate
“People say they are afraid that if their private information becomes known, they may not be able to get health insurance.”
– Dr. Farzad Mostashari, National Coordinator for Health Information Technology
The first civil penalty levied under the HIPAA Law: 41 patients could not access files
This is an example of a case where the health insurance denied patient’s right to view their own records. Cignet Health of Prince George’s County Md. has been charged 4.3 million dollars as civil penalty for denying accessibility to 41 patients to their medical records. For more information on this story.
A pre-existing health condition should not discriminate any citizen from obtaining health insurance, but there is legitimate fear that if patients’ private health records are open to entities that do not have to follow HIPAA, they will be vulnerable to prejudice.
These are the entities that are not required to follow HIPAA:
- life insurers
- employers
- workers compensation carriers
- many schools & school districts
- many state agencies like child protective service agencies
- many law enforcement agencies
- many municipal offices
The adoption of EMRs is critical to the telemedicine cause. It’s imperative that these violators from “The Wall of Shame” be publish and held responsible for violating HIPAA. Due to the The Health Information Technology for Economic and Clinical Health act or the HITECH Act (under HIPAA) the Secretary of Health & Humans Resources much post all violators of 500 patients or more.
 The Department of Health and Human Service website exposes 281 Health Insurance Portability and Accountability Act (HIPAA) security violations that affected more than 500 individuals as of June 9, 2011.
The Department of Health and Human Service website exposes 281 Health Insurance Portability and Accountability Act (HIPAA) security violations that affected more than 500 individuals as of June 9, 2011.
Privacy, Security & Confidentiality (HIPAA)
In order to guarantee patient security, privacy and confidentiality the department of Health and Human Services created HIPAA to streamline the process of create Electronic Medical Records (EMR). The adoption of EMR (which involves telehealth) is critical for telemedicine. 
“People need to be assured that their health records are secure and private. I feel equally strongly that conversion to electronic health records may be one of the most transformative issues in the delivery of health care, lowering medical errors, reducing costs and helping to improve the quality of outcomes.”
– Kathleen Sebelius, Secretary of Health and Human Services
Our health information is protected under federal law. The following entities must follow HIPAA:
- Health Plans, including health insurance companies, HMOs, company health plans, and certain government programs that pay for health care, such as Medicare and Medicaid.
- Health Care Providers—those that conduct certain business electronically, such as electronically billing your health insurance—including most doctors, clinics, hospitals, psychologists, chiropractors, nursing homes, pharmacies, and dentists.
- Health Care Clearinghouses—entities that process nonstandard health information they receive from another entity into a standard (i.e., standard electronic format or data content), or vice versa.
Benefits to telemedicine
- Improved Access – Bringing healthcare services to patients in remote locations.
- Cost Efficiencies ‐Telemedicine has been shown to reduce expensive hospital visits from chronic diseases. Online electronic medical records would increase productivity by having medical records on “the cloud” and multiple copies do not have to be replicated. Patients are monitored at the their own home environment.
- Patient Demand ‐ According to the American Telemedicine Association, patients want telemedicine. The ability to reduce travel time and cost of travel would increase comfort by staying at home.
- Government
- Hospitals
- Rural Telemedicine
- Home Telehealth Care
- School Telehealth
- International Telemedicine
- Telepharmacy
- Disaster Telemedicine
- Telelearning
- All Medical Specialties
What is telemedicine
What is Telemetry:
Telemetry is the science and technology of collecting sensor data and transmitting it to a remote location. Remote monitoring, in essence, is the ability to ‘see’ and sometimes control from a distance. Telemedicine is just an application of this growing field.
“Telemedicine is the use of medical information exchanged from one site to another via electronic communications to improve patients’ health status. Closely associated with telemedicine is the term “telehealth,” which is often used to encompass a broader definition of remote healthcare that does not always involve clinical services. Videoconferencing, transmission of still images, e-health including patient portals, remote monitoring of vital signs, continuing medical education and nursing call centers are all considered part of telemedicine and telehealth.” (via American Telemedicine Association)
Studies have shown that patients support telemedical services. Telemedicine offer patients access to care that might not be available otherwise as well as medical services due to distance.
Fear of adopting EMR: Is it for good reason?
Are you worried about LULZSec or Anonymous hacking the Cloud and going after your health information?
You really shouldn’t be.
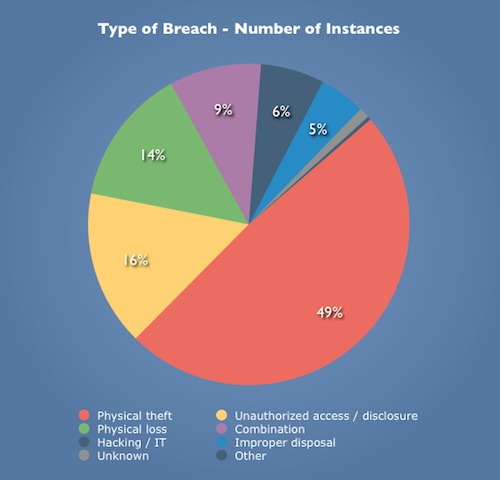
As demonstrated by “The Wall of Shame” pie chart illustrated below, almost 50% of the security breaches are due to carelessness. Michael Koploy states: “Overall, physical theft and loss accounted for about 63% of the reported breaches. Unauthorized access / disclosure accounted for another 16%, while hacking was only 6%.” As Koploy states, do you really think hackers would rather seek your HDL/LDL cholesterol count or a bank account. (Good point!)
- 6,800 paper records that were supposedly mailed but never received
- an impostor posing as a recycling-service employee stealing over 1,300 individuals’ records and films; and,
- a laptop stolen by a former employee that contained personal health records of over 50,000 patients.
Read more here.
Once you realize how so many of these security breaches could have been avoided combined with the realization that doctors also love their mobile computers/laptops/smartphones, the statistics of security breaches become very real. There are 10,000 mobile health care apps that allow users to access EMRs and according to Mobile Marketing Watch, one in three doctors own an iPad, and another 28% are planning on buying one within the next six months. Within the past two year there have been 116 data breaches of over 500 records due to the theft or loss of mobile devices. We really need to have more stringent safe guards, not only training of the health care professionals, but as the FCC and FDA work together as the convergence of technologies deal with new health care apps there needs to be better protection for the consumers. The Wall of Shame isn’t going to disappear unless the government and the people come to terms with their health care records being exposed.
Here are 8 tactics for mobile data privacy & security (via Mary Mosquera of GovHealthIT )
1. Don’t store sensitive data on wireless devices. If required, encrypt data.
2. Enable password protection on wireless devices and configure the lock screen to come on after a short period of inactivity.
3. Turn on the “remote wipe” feature of wireless devices.
4. Enable Wi-Fi network security. Do not use wired equivalent privacy (WEP). Wi-Fi protected access (WPA-1) with strong passphrases offers better security. Use WPA-2 if possible.
5. Change the default service set identifier (SSID) and administrative passwords.
6. Don’t transmit your wireless router’s SSID.
7. Only allow devices to connect by specifying their hardware media access control (MAC) address.
8. Establish a wireless intrusion prevention system.